Humphrey wishes to share his experience, and hopes he won't have to go for a fourth round (but you never know - and we'll do better next time). Here, he rounds up lessons learned in terms of treatment and recovery, as well as the financialization of them.
If you're new to corneal lesions, be cautious, but don't panic! While they can be dangerous, if the ulcer is not too deep, there's a pretty good chance of full recovery. Once the ulcer heals, it can take a while (even months) for the scar tissue to resolve. But usually, sight is eventually fully restored.
1. When to go to the vet for a suspected corneal ulcer
Squinting can indicate the first signs of an ulcer - squinting often implies eye pain. Humphrey was squinting, but also a cloudy, gray "dot" appeared on his eye - which is really bad! Excessive tears or discharge can be another sign. That usually suggests an infection. If these symptoms are present, it's not a bad time to take a dog to the vet!
To determine if the cornea is damaged, the vet will have to do a fluoroscien stain - where fluorescent dye is put on the eye to show a lesion or wound, because they normally aren't visible to the naked eye. It the tear is bad (see below), a vet may make a referral to an ophthalmologist.
2. Types of corneal ulcers: the not-good, the bad, and the ugly
Humphrey has noticed that ulcers are assessed along a couple of axes: depth, and infection.
First, there's the depth of the ulcer. The cornea is a transparent surface covering the eye - but it is made up of 4 layers (which I also described in a previous post), which you can see in the image below (source).
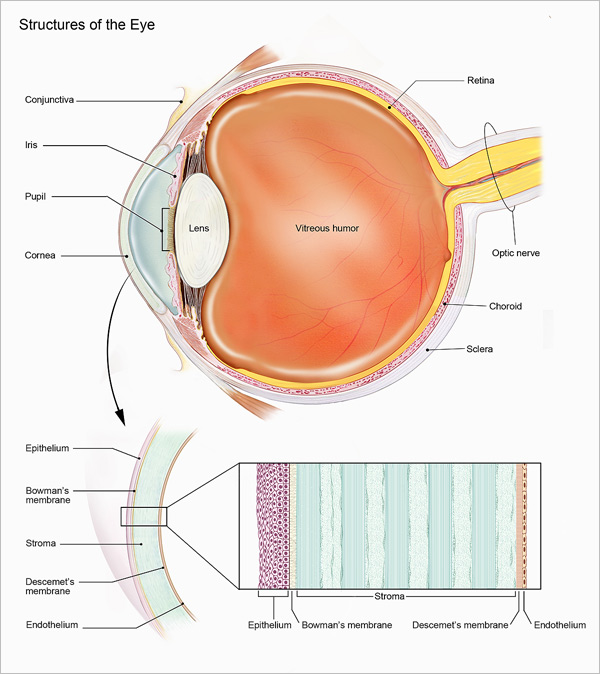
Humphrey has had 2 stromal ulcers (one in each eye) in the past 4 weeks, meaning that the depth was beyond the epithelium and Bowman's membrane. The deeper the ulcer the more dangerous it is - and the longer it takes to heal. His superficial ulcer (which was only the epithelium) healed in about a week, his first stromal ulcer took a little less than 3 weeks to fully heal. The second stromal ulcer is a work in progress, but has shown signs of very good healing without CXL (but with more frequent drops) within 2 days. To Humphrey's untrained eye, this one is healing much faster than the first one, and with a lot less discomfort.
In addition to the depth of the ulcer, an ophthalmologist will note if the ulcer is infected - the problem with an infection is that it eats away at the corneal tissue and prevents healing. This is called a melting corneal ulcer. Humphrey has had 2 of these! The ophthalmomogist might use terms like "malacia" or "actively dying tissue" (which appeared in Humphrey's documentation). The danger is permanent loss of corneal tissue, and the worst case scenario is corneal perforation - where the infection eats away the entire cornea! This can happen quickly with a bad infection (some reports say as quickly as a day or two). So far Humphrey has managed to catch his melting corneal ulcers in time, and prevented tissue loss deeper than the stroma.
3. Triage: Initial treatment
Different ophthalmologists have different approaches to triage and early treatment of corneal ulcers.
In Humphrey's first experience, Corneal Crosslinking (CXL) was strongly advised to kick-start healing. The problem with CXL (which is used in humans and dogs) is that how much the eye benefits is not truly known. It will definitely not harm the eye - because all it involves is adding a lot of collagen in the form of riboflavin to the eye surface over about 20 minutes, then shining a special light on the eye. CXL is an emergency-type triage treatment and is followed by more conventional drop therapies to promote healing and stop infection. The other problem with CXL: it is (perplexingly - since it's so simple and done by vet techs) very expensive: $1200 in Toronto.
For Humphrey's second stromal ulcer, he saw a different ophthalmologist, who said she does not do CXL at all, because the evidence to support it is insufficient. "It's an adjunct therapy," she said. So the first course of treatment was drops every 2 hours.
 |
| That wink looks adorable, but it's actually Humphrey's discomfort when he had his first corneal ulcer! |
4. Managing healing to recovery
All three of Humphrey's ophthalmologists put him on therapy with drops, with very slight variations in content, and different schedules. The first ophthalmologist had Humphrey on atropine drops for pain once daily, and two antibiotics (Tobrex, Vigamox) plus plasma every 6 hours for 3 weeks. Healing was noted in a week, and the drops were continued for a total of 3 weeks.
The second ophthalmologist had Humphrey taking one antibiotic (Vigamox) and plasma every 2 hours for 3 days, then every 4 to 6 hours thereafter. The frequency was reduced only after a fluoroscien stain indicated improvement. Instead of a topical pain reliever (atropine), this vet prescribed an oral pain killer (tramadol) as needed. That second vet also recommended Opixcare eye lubricant, which seems to make a big difference in his comfort (Humphrey asked about a lubricant from the first vet because his eyes are always on the dry side, but was told it was not necessary).
Even in human medicine, the frequency of drops recommended by ophthalmologists seems to vary. Some reports suggest hourly plasma for the first couple of days, others every 2 hours, and others every 4 hours.
Antibiotics are important to eradicate the infection, and plasma promotes healing. For Humphrey, the plasma serum (which is actually plasma ophthalmologic serum that probably contains saline) comes from an animal blood bank. Plasma has been used in human and veterinary ophthalmology for about 20 years with great results - it contains enzymes that promote healing, tends to reduce inflammation and has no side effects in most users. Humphrey was told he can use it as often as he wishes.
The order of drops matters: plasma first, then antibiotics, then lubricant. As well, all the vets Humphrey consulted ordered at least 5 minutes between drops. And all ordered that the area around the eyes be kept free of debris (which means very, very gentle wiping with a cotton pad or compress).
Humphrey experienced a bit of confusion on how long to use thawed plasma serum (it is dispensed frozen). One vet said 2 to 3 days, another said up to a week. Extensive online research suggests that older advice was 2 to 3 days, but more recent studies on the degradation of plasma claim that so long as it's always kept refrigerated, it can have therapeutic benefits for about a week (though YMMV!).
Be sure to get an appropriate cone that will prevent rubbing against the cone itself, as well as protect the eyes from debris. Two of Humphrey's three vets also said RexSpecs (see below!) are appropriate, but not Doggles. RexSpecs take a little getting used to, so it's not a bad idea to train a dog to wear them when they are young and healthy.
If corneal ulcers do not heal on their own, or if they are very deep (deeper than Humphrey's), surgical options exist, and apparently have high degrees of success. Solutions include corneal grafts and transplants. If a problem with the eye area (for example, inward-turning lashes) causes repeated ulcers, some can be surgically corrected to prevent further injury.
5. How to save a few bucks in buying supplies and selecting treatment
The best advice Humphrey can offer is to get multiple ophthalmologic opinions if you can afford it, and ask a LOT of questions. Sadly, sometimes you get no answer to a question, or competing advice (as with CXL). Then you have to make a choice.
Given that Humphrey's second ulcer healed fairly rapidly without CXL, he would not repeat this procedure, which would save $1200. The 2-hour frequency of drops worked well for him, though obviously poses a burden on caregivers.
Always price check medications! Humphrey could have saved hundreds of dollars by taking prescriptions to his local pharmacy. For example:
- Humphrey was charged $77 for compounded atropine, which was $17 at Shopper's drug mart
- Humphrey was charged $40 for generic Tobrex, $25 at the human pharmacy, and only $14 at the Toronto veterinary pharmacy!
- Humphrey was charged a whopping $70 US for generic Vigamox, which was $25 CD or $29 US at the pharmacy. Twice!
- Humphrey was charged $40 US for Optixcare eye lubricant which is $14 at the Toronto pet pharmacy without a prescription
- The cost of plasma serum varied between $50 US and $75 CD. The $50 amount was greater volume, but in a single dispenser which had to be discarded, whereas the $75 set was 5 loaded syringes that could be defrosted as needed and reduced waste. This cannot be filled in a conventional pharmacy!
 |
| Hundreds of dollars of drops, and syringes filled with plasma serum! |
Obviously, having to fill prescriptions at the pharmacy means extra trips, and delays the start of drops until picked up. But veterinarians in Ontario cannot deny a written prescription request (the Veterinarians Act RSO 1990 states this), so patients have every right to request this approach, bearing in mind some veterinary preparations need to be filled from a veterinary pharmacy and cannot be obtained at the human pharmacy, and vice versa for some of the antibiotics.
6. Possible Underlying Causes of Chronic Corneal Lesions
While corneal lesions and ulcers can occur through trauma (scratching the eye while sniffing around a bush with many branches), some dogs have underlying conditions that lead to frequent lesions and ulcers. Dr. John Sapienza created a thorough and easy to follow explanation of corneal ulcers and some of the underlying causes. They include:
- Defects in the basement membrane of the cornea, which can either be treated with plasma or surgically
- Chronic dry eyes (Keratoconjunctivitis Sicca), which can be treated with topical cyclosporine (Restasis)
- Chronic superficial keratitis (or CSK) in which the cornea is inflamed, and can be treated with topical steroids or topical cyclosporine
- Corneal degeneration, which can be treated with lubricants that improve the tear film, cyclosporine (to improve the tear film and to provide immunomodulatory function), EDTA (to bind to the calcific material), and topical antibiotics to fight infection. Surgical options include a superficial keratectomy to remove degenerative material, conjunctival grafts to provide support, excimer laser ablation of the lesions, corneal cyanoacrylate application, and donor corneal transplants. Note that EDTA is a non-invasive choice in people and dogs, and has been used for many years with good results
- Episcleritis, or the inflammation of the tissue underlying the conjunctiva and overlying the sclera
- Corneal neoplasia, or tumours
No comments:
Post a Comment